Immune checkpoint inhibitors: brave but flawed heroes in the battle against cancer
With longer lifespans and improved diagnostics, the chances of any of us being diagnosed with cancer during our lifetime are significant. Flip a coin, if it’s heads… Those are the odds. Some diagnoses may feel scary but have very high survival rates (95–99%), especially when detected early. These include thyroid, prostate, and early-stage skin cancers like melanomas. Other cancers, such as those of the pancreas, brain, and lung, are sadly much more serious. However, we must not avert our gaze from the reality of cancer and the battle against it, especially since progress in cancer survival rates over the last decades has been astounding.
Today I'm exploring a 2023 review paper on cancer immunotherapy with immune checkpoint inhibitors. We're going to examine:
What immune checkpoint inhibitors (ICIs) are and how they work
Their effects on reversing the course of metastasised cancers - those where cancerous tissue has spread to secondary locations via the bloodstream
Innovations in delivering treatments for brain cancers despite the presence of the blood-brain barrier (BBB)
Essential Terms and Concepts
Antibody:
A protein produced by:
B-cells residing in lymph nodes
Mucosal tissues in the gut and respiratory tract
Size: Antibodies are similar in size to enzymes like lactase, which breaks down lactose, and are approximately 2.5 times larger than haemoglobin, the molecule that can carry up to eight atoms of oxygen. Side note on haemoglobin: it's composed of roughly 15,000 atoms to carry eight oxygen atoms.
Function: Antibodies bind to a specific protein expressed on a cell surface. By binding to it, they change their conformation to expose a receptor that immune cells recognise as a tag to engulf the antibody-tagged cell.

Antigen (mnemonic: "antibody generator"):
Anything that may trigger an antibody response. In the context of this article, cancerous tissues will present on their surface mutated proteins that are "non-self" - neo antigens. Sometimes they will present "self" proteins that are not mutated but over expressed, meaning there’s more of them on the cell surface as well. This also may trigger an immune response.
Mechanisms of tumour detection
All cells present on their surface small 8 to 11 amino acid long sequences - peptides - for immune surveillance. They come from recycled proteins previously inside the cell’s body. A regular cell will only present sequences that are known to the immune system. Cells that begin to express mutated proteins inside them, or cells infected with foreign viruses causing them to produce viral proteins, will "smell funny" to the immune system by expressing unknown short peptides. Quick maths: there are 10 trillion combinations of 10 long amino acid sequences.
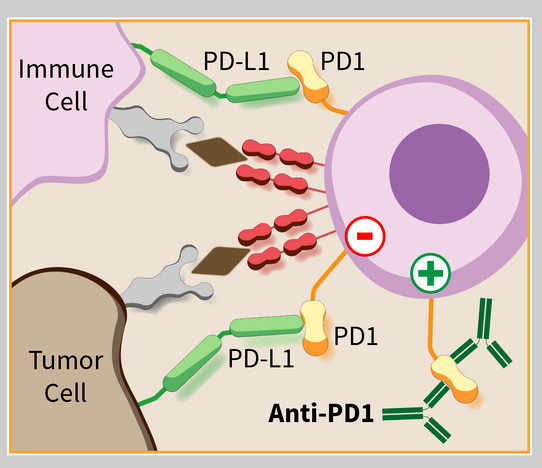
T-cells which patrol the body also express proteins on their surface. Full proteins, not tiny peptides. One highly investigated protein on the T-cell's surface is called PD-1. When a complementary protein, PD-L1 (L for ligand), binds to PD-1, it deactivates the T-cell. In a normal scenario, PD-L1 will be increasingly expressed on healthy cell surfaces following an increase in T-cell populations to downregulate their activity and prevent autoimmunity. That's the inhibitory checkpoint to keep the immune system in balance.
Many cancers express PD-L1 on their cell surface to bind to PD-1 on T-cells, thereby deactivating them. Although PD-1 is one of many proteins that have this function, and cancers may have complementary counterparts, it is sufficient for us to focus on PD-1 to explore antibodies and their function as immune checkpoint inhibitors - sounding the bugle call for another charge against cells that express PD-L1. Some of these happen to be cancer cells.
Fighting metastasis
Localised treatment of tumours is no longer possible once the cancer begins to spread via the bloodstream or other avenues: nerves, lymphatics, neighbouring tissue, and others. Chemotherapy and ICIs are then therapies of choice. Different checkpoint proteins silence T-cells for different cancers. For some, even after metastasis, it is possible to win the war through correct identification and preparation of a matching cocktail of monoclonal antibodies, which enable the immune system to wipe out tumorous tissue.
Blood-Brain Barrier
I must admit that I always thought the blood-brain barrier (BBB) only allowed very small molecules like oxygen, glucose, and certain hormones to pass through. It did not occur to me that it's possible to create large molecules that can pass through the BBB with the aid of helper proteins.
The review article cites two methods of transmitting treatment cargo through it.
Even with hormones, I was wrong. They are too large to simply diffuse through the membrane. Insulin, leptin, and other substances are transferred via their respective receptors in a process called transcytosis—which literally means "across the cell." In this Trojan horse technique [link to the paper that the review cites], a drug is coupled to a monoclonal antibody that is directed against one of the BBB's transcytosis receptors allowing passage.
Apart from hormone passage receptors, transferrin - which serves the iron-hungry brain - can be targeted with a matching antibody delivered inside a small fatty vesicle, a liposome.
Ultrasonic blasts to BBB
In patients with brain cancers (glioblastomas), caused by astrocytes - a type of glial cell - turning cancerous, radical treatments disrupt the blood-brain barrier with ultrasound(!). Quote: "Low-intensity pulsed ultrasound (LIPU) was utilised in a recent Phase I/IIa clinical experiment to damage the BBB and let a medication enter the brain. During the trial, patients had the SonoCloud-1 device implanted into their skull bones so that pulsed sonication could be administered. The research revealed that patients tolerated LIPU well and that carboplatin (a chemotherapeutic) could penetrate the brain after being sonicated."
Job not done
While in some cancers ICI treatment may result in up to half of patients responding, many develop resistance to ICIs often after a few months. Sadly, the precise mechanisms of this resistance are not well understood. It will be explored further next week.



